CHIBE and Humana Discuss Changing Care Models in the 21st Century
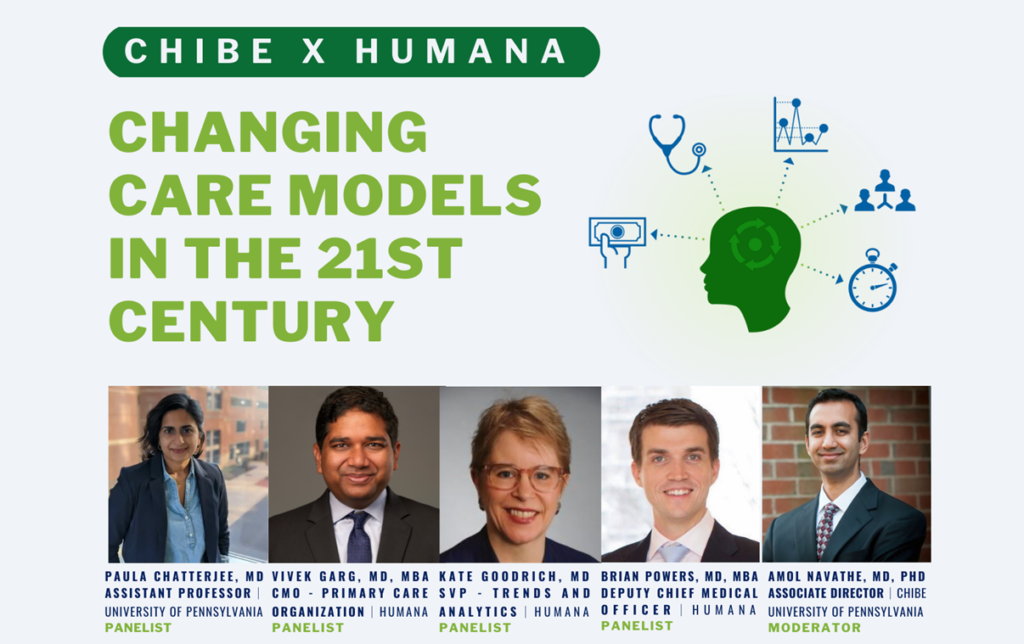
Penn’s Center for Health Incentives & Behavioral Economics (CHIBE) hosted a webinar on March 29, 2022, with panelists from the University of Pennsylvania and Humana to discuss how health care is evolving and how we might optimize the value of care received to improve patient outcomes, address health equity concerns, and make care more affordable.
See excerpts from the panel event, moderated by CHIBE Associate Director Dr. Amol Navathe, below, and watch the recording here.
On the Evolution of Primary Care and What It Will Look Like in the Future
Dr. Vivek Garg, Humana’s Chief Medical Officer, Primary Care Organization, sees significant progress being made in primary care and believes that patients will have much more choice in how they receive primary care and who they receive it from in the future.
“There’s a key question here, though, that people will face: Is primary care a bundle of services or is it a relationship with someone or a team who knows your context and needs and can help you in your health journey? When you look at virtual care and retail sites of care, I think that tension will be front and center and has yet to be answered in terms of whether these more limited service providers can really meet the full intent of primary care.”
Dr. Garg talked about the importance of “purpose-built care models” in primary care, which are specifically designed for the needs of a distinct population. Humana’s primary care model, through CenterWell and Conviva, addresses the most important physical, emotional, and social needs of seniors through a physician-led care team in community-based centers, with programs in care management, behavioral health, transportation, pharmacy and more. Other models address populations such as women and children or people living with specific conditions, such as diabetes.
“People vote with their feet, and we still need to see where they will seek care,” he said, noting that many patients want a longitudinal relationship and some may want to self-manage their care.
On Specialized Primary Care Models and Unintended Effects
Dr. Paula Chatterjee, Assistant Professor at the Perelman School of Medicine, talked about the risk of hyper-specialization of different types of health care providers and what effects that may have on patients.
“You see that the patients who are often most able to access those specialty care services are the ones who are often most savvy to begin with,” she said. “They have built relationships with the health care system. They have relationships with multiple different providers, so that they’re able to be funneled into places that are really good at what they do, and while that’s of course valuable … there’s always a risk of leaving behind those who are already unable to access services to begin with. I think what this comes down to is a bit of a measurement problem. So much of health and equity right now is rooted in what we choose to measure, and we miss a lot in what we are unable to measure. So, oftentimes, the patients that we are most trying to reach are the ones we’re not seeing in our claims, and we’re not seeing in our data, because they have so many barriers before they even show up and present. How do we measure who we are missing? And then how do we make sure that they have the relationships in place, the connections to existing health care providers, so that they can capitalize on the benefits of where future innovative care delivery is going to be?”
On Telemedicine and Who May Be Left Behind
Dr. Chatterjee saw telehealth as a powerful tool in both urban and rural areas during the pandemic, and what helped with scalability was the speed of how fast the payment system was figured out.
“Now that we have some time and some evidence, we’re able to see where telemedicine worked well and where it didn’t … Over 70% of the US population have access to broadband, for example, but the 25-30% that don’t are the ones who are already made vulnerable by a variety of other structural factors, and they already bear the brunt of health disparities. I think that telemedicine has a lot of potential promise, but I think we have to bundle it in with concrete decisions about payment as well as concrete polices, whether at the state level or the federal level, to increase broadband access.”
On Payment As An Enabler for New Care Models
Dr. Brian Powers, Deputy Chief Medical Officer at Humana, said new care models need time, energy, and investment.
“You need resources to invest, and you need to be able to share in the savings from better care to reinvest. I think it’s unreasonable to expect primary care to do more with less or to do more with the same. Our priority at Humana has been to have as many of our members see a primary care physician in a value-based payment arrangement,” Dr. Powers said.
Evidence shows that Humana’s members who see value-based primary care providers have better health outcomes, better medication adherence, and better access to chronic and preventive care. Last year, they saw 67% of their Medicare Advantage members in a value-based payment model with accountability for total cost of care.
Dr. Powers credited their success to working closely with providers, sharing data with them, and helping them understand the levers that they can pull on to perform well. He shared that physicians in value-based contracts also earned more of the overall health care dollar, too, compared with those in fee-for-service models (roughly 18 cents vs nearly 7 cents of the health care dollar).
Metrics in Care Models
Dr. Kate Goodrich, Senior Vice President of Trend and Analytics at Humana, highlighted the importance of getting the right metrics to drive behavior change and thinking about what the problem is that the model is trying to solve and then centering the metrics on that. In addition, there should be shared accountability for performance on metrics and meaningful financial incentives tied to performance on the metrics as well.
“As we’re thinking about implementing any new type of payment arrangement or new program, we need to be thinking up front about the way we’re going to understand whether it’s working and do that in a rapid, iterative fashion,” Dr. Goodrich said.
She added that equity should be a critical component of the measurement strategy and to be sure to hold providers accountable for improving performance on that metric over time.
Closing Thoughts
Dr. William Shrank, Chief Medical Officer at Humana, concluded the session by talking about the importance of looking at these issues holistically.
“In order to deliver on the outcomes that we’re trying to promote in the setting of value-based care, we need to leverage better technology, and we need to be able to understand the populations we serve, as Kate focused on. We need to be able to measure in real time how we’re performing and how we’re designing and developing clinical programs to meet the needs of our members and our patients, as Paula noted. We need to make sure that our members and our patients have access to the technology that allows them to be better engaged through better broadband access. And as Vivek really highlighted, the answer is not that everyone needs primary care; it’s really what is in that primary care relationship that makes it meaningful. It is a relationship. It’s more than just a set of care packages or care pathways.”