Dr. Kevin Volpp Testifies Before Senate Subcommittee on ‘Food as Medicine’

CHIBE Director Kevin Volpp, MD, PhD, appeared before the Senate Committee on Agriculture, Nutrition, and Forestry’s subcommittee on food and nutrition on December 12 to talk about the connection between chronic disease and nutrition and to call for continued federal support for nutrition research and “Food as Medicine” programs.
Senator Cory Booker, chairman of the subcommittee, opened the hearing highlighting some of the consequences that unhealthy, processed diets lead to—for example, half of Americans have diabetes or prediabetes and half of all children today are estimated to be obese by the time they turn 35 years old.
“The effects of diet-related diseases are not limited to the health care field. They are causing an economic crisis that is spiraling out of control,” said Senator Booker, citing that health care is 20% of the country’s GDP.
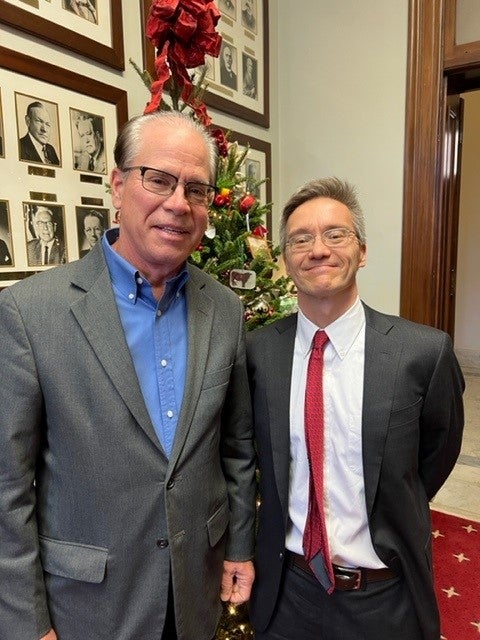
“A lot of what ails our health care system is overutilization because we’ve never changed the lifestyles that take us into the health care system in the first place, and that starts with your diet,” said Senator and Ranking Member Mike Braun, who invited Dr. Volpp to serve as a witness at the hearing.
Dr. Volpp appeared as a witness on behalf of the American Heart Association (AHA). Dr. Volpp is the leader of the planning committee for The Rockefeller Foundation and American Heart Association’s “Food is Medicine” Research Initiative, as well as a volunteer member of the AHA’s Advocacy Coordinating Committee. He is also the Mark V. Pauly President’s Distinguished Professor at the Perelman School of Medicine and Wharton at the University of Pennsylvania.

In his testimony, Dr. Volpp cited that cardiovascular disease is the leading cause of death in the United States and accounts for 12% of total U.S. health expenditures. Heart disease and stroke cost the health care system $216 billion annually and cause $147 billion in lost job productivity. One key element that contributes to chronic disease and cardiovascular disease is unhealthy diets, and this issue is especially important for lower-income individuals and people of color – communities where healthy food is often less accessible.
“The connection between chronic disease and nutrition is undeniable,” Dr. Volpp said. “Our diets not only play a role in our risk of developing chronic diseases, but also can prevent, manage, and treat these diseases. Stable availability, access, affordability, and use of nutritious foods across the lifecycle can help reduce the risk of chronic diseases and help treat and manage chronic diseases. Unfortunately, many individuals in the United States are nutrition- and food-insecure and do not have access to affordable, nutritious food. There is a growing body of evidence that the health care system can be utilized to help patients access and consume healthy foods. To help address unhealthy diets and nutrition insecurity, evidence-based, cost-effective nutrition and food programs can be integrated into the health care system.”
Two examples of the “Food is Medicine” concept are 1) medically tailored meals, which involve home delivery of meals prepared by registered dieticians — especially helpful after patients are discharged from the hospital after an event such as congestive heart failure — and 2) healthy food prescription programs, where providers “prescribe” healthy food to patients by offering coupons or vouchers for farmers’ markets, grocery stores, or mobile markets. Dr. Volpp noted there is research demonstrating how these two approaches have been associated with improved health outcomes for patients with chronic diseases, but that there is a lot of work to do to answer important questions about intensity, duration and delivery of such programs; the role of educational strategies or coaching in helping people change habits; incorporation of patient preferences and about cost effectiveness.
“The research must be designed to help decision-makers across the country—by creating private public partnerships that facilitate testing of ways to increase access to healthy food and sharing of data that facilitate analysis,” Dr. Volpp said.
A key question is whether programs can be developed that are sufficiently cost effective to merit benefit coverage and reimbursement for patients.
Dr. Volpp also highlighted that a new initiative is set to launch in spring 2023 that will help inform how the health sector can design and scale programs that increase access to nutritious food; the Rockefeller Foundation and the AHA are putting $250 million to work to build this national “Food is Medicine” Research Initiative.
“Chronic diseases and unhealthy diets are inextricably linked, and health disparities remain all too pervasive,” Dr. Volpp concluded. “Continued federal support for nutrition research, including ‘Food is Medicine’ programs, will be necessary to support efforts to prevent and treat chronic diseases, lower health care costs, and improve quality of life.”
Click here to watch Dr. Volpp provide testimony at this meeting around the 54:50 mark. His written testimony is also available to download on that page. Find media coverage from MedPageToday here: ‘Whole-of-Government’ Approach Needed for Diet-Related Illnesses, Senator Says.