The ASCVD Risk Reduction Initiative
Atherosclerotic cardiovascular disease or ASCVD is the leading cause of morbidity and mortality in the United States. What makes this high disease burden particularly frustrating is that many of the preconditions like hypertension and hyperlipidemia are often easy to diagnose and have safe and effective treatments. With perfect adherence, low-cost cardiovascular drugs could reduce cardiovascular events by 62-88%, highlighting the opportunity to reduce ASCVD risk through translation of known treatments. However, only about 1 in 4 adults nationally with elevated ASCVD risk have well-controlled lipids and about half have well-controlled blood pressure.
Conventional approaches to broad population care gaps often include layering more responsibility on primary care clinicians, sometimes with financial incentives for clinical targets but often with little practice support to facilitate reaching those targets. Given that primary care clinicians have high and increasing levels of burnout, improving population health may be better achieved by providing operational support so primary care clinicians can do less rather than financial incentives to encourage them to do more.
About the ASCVD Initiative
Given the health and economic benefits of reducing ASCVD risk and the challenges of achieving them by giving primary care clinicians more to do, we launched the ASCVD Risk Reduction Initiative in June 2021. The ASCVD Risk Reduction Initiative is improving the ways that primary care clinicians help patients with ASCVD and those at higher risk of ASCVD improve their heart health. Our flagship program is Penn Medicine Healthy Heart, an innovative care delivery model for heart disease risk reduction.
The Initiative is funded from the National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) Program through the Perelman School of Medicine Institute for Translational Medicine and Therapeutics. The Initiative is also supported by funding from Penn Medicine.
Our flagship program: Penn Medicine Healthy Heart
The initiative’s flagship program is Penn Medicine Healthy Heart, an innovative care delivery model for heart disease risk reduction.
With support from the NIH Clinical and Translational Science Award and institutional support from Penn Medicine, Penn Medicine Healthy Heart is a 6-month program grounded in behavioral economics insights to increase the uptake of and adherence to evidence-based interventions to reduce ASCVD risk.
This text-based program is being offered to approximately 2,000 Penn Medicine primary care patients in West and Southwest Philadelphia and Lancaster County in 2024-2025 as part of a clinical trial to evaluate its effectiveness, cost effectiveness, and implementation. The goal is to help patients take action to reduce their heart disease risk by lowering their blood pressure and cholesterol from home while providing additional resources to our busy primary care providers.
Penn Medicine Healthy Heart emphasizes proactive outreach and prevention outside of a traditional visit model using data assets to identify and risk stratify patients. The program offers blood pressure monitoring and management, cholesterol counseling and medications, healthy eating resources including a custom video series on heart healthy eating, and smoking treatment to patients via text, phone, and video.
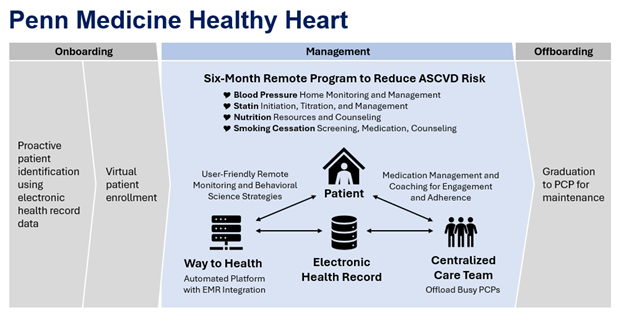
The program also aims to relieve overburdened primary care providers through automated hovering technology coupled with a centralized, leveraged team of non-clinical navigators and nurse practitioners.
Penn Medicine Healthy Heart was developed over two years through more than 15 pilot projects across Penn Medicine. One notable pilot study found a way to drastically increase statin prescribing rates for patients who would benefit from them. (Statins are prescribed to patients who have a high risk of ASCVD to lower their risk of heart disease and heart events.)
Instead of relying on doctors to assess a patient’s cardiovascular risk and determine whether a statin is needed and at what dose – a process that physicians may not have adequate time for during a patient’s visit – this pilot study investigated automated referrals to pharmacy services. Pharmacists contacted the patients, discussed the use of statins, and initiated therapy when appropriate.
The researchers discovered that around 86% of the eligible patients were not prescribed statins at baseline, and others were receiving a dose that was too low.
Patients in the intervention arm who had automated referrals had a significant boost in statin prescription rates – 31.6% were prescribed a statin compared with around 15% in the usual care group. The researchers also found that nearly 25% of the patients in the intervention arm were prescribed a statin at the guideline-recommended dose during the study period compared with 7.7% of patients in the usual care group.
Overall, the research team found that the odds of prescribing the appropriate dose of statins increased sixfold when automated referrals were made to pharmacy services.
Find publications and media coverage below:
Collaborators
PI Oversight Committee
Kevin Volpp, MD, PhD (Project PI)
David Asch, MD, MBA
LauraEllen Ashcraft, PhD, MSW
Alexander Fanaroff, MD
Karen Glanz, PhD, MPH
Shivan Mehta, MD, MBA, MSHP
Matthew Press, MD, MSc
Mary Putt, PhD, ScD
Louise Russell, PhD
John Wood, MD
Program Leadership
Laurie Norton, MA, MBE, Senior Research Director
Kayla Clark, MPH, Project Manager
Marguerite Balasta, MD, Medical Director
Jingsan Zhu, MS, MBA, Analytics Director
Wendell Kellum, MD, Informatics Lead
Executive Council
Thomas Cappola, MD, ScM
Deborah Driscoll, MD
Garret FitzGerald, MD, FRES
Kevin Fosnocht, MD, FACP
C. William Hanson, II, MD
Judith Long, MD
Raina Merchant, MD, MSHP
Dan Rader, MD Richard Wender, MD